Medicine in Crisis
Reducing the pressure on A&E
In the context of increased pressures on A&E Departments across the UK and the Government?s promise of introducing a seven-day GP service by the end of this parliament, we asked a sample of 2,003 UK adults about their hospital visits over the past year. As this article will explain, our results would suggest that the simple introduction of seven-day GP services is unlikely to reduce the pressure facing A&E Departments, unless it is accompanied by generational change that combines education with technological innovation around how health services are delivered.
Our findings were surprising to say the least. Contrary to the widely held belief that the pressures facing Emergency Departments are being generated by an increasingly aged society, our findings demonstrate that the most frequent users of A&E are those aged 34 and under. Nearly half (47%) of those aged 34 and under have attended A&E in the past year compared to just 25% of those aged 55 or over. Moreover, a quarter of those aged 34 and under have attended A&E more than once in the past year compared to just 10% of those aged 55 and over.
When we investigated the reasons for each visit, we saw that for those aged 55 or over the causes were broadly in line with what one might expect. Nearly a third (30%) of respondents stated that their symptoms were related to a pre-existing health problem, such as headaches following a previous tumour or chest pain following a previous cardiac episode. The next most common causes were collapses or falls and dislocations or fractures, both of which tend to increase in frequency as people get older.
For those aged 34 or under, the most common cause of visiting A&E was to treat a minor injury (such as a cut or laceration) with 21% stating this as their primary symptom. (Nearly twice as many men visited A&E with a minor injury than women ? suggesting that the weekend football pitch is a dangerous place to be.) However, outside of minor injuries, we start to see disturbing patterns in the causes of visits. Nearly one in ten visits are driven by drug or alcohol related injuries compared to 1% for the rest of the population. Over one in ten (14%) visits are driven by head injuries or gastric discomfort (described in our survey as a stomach ache). Finally, a further 14% of visits are caused by cases of cold, flu or fever ? for which 0% of those aged 55 and over visited A&E.
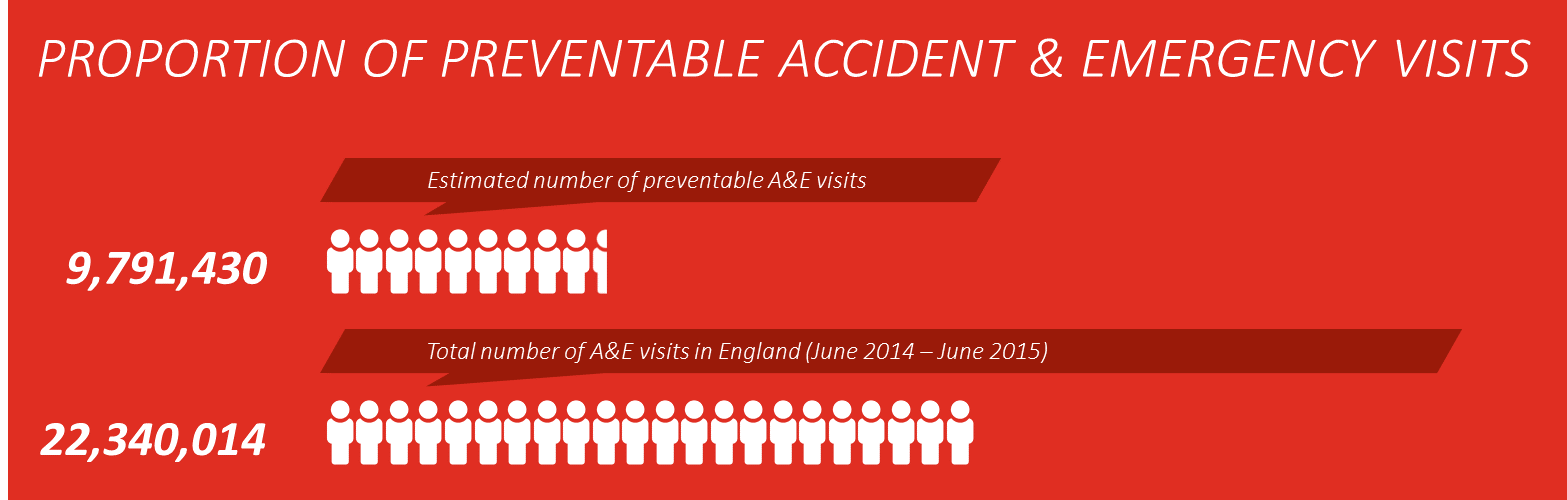
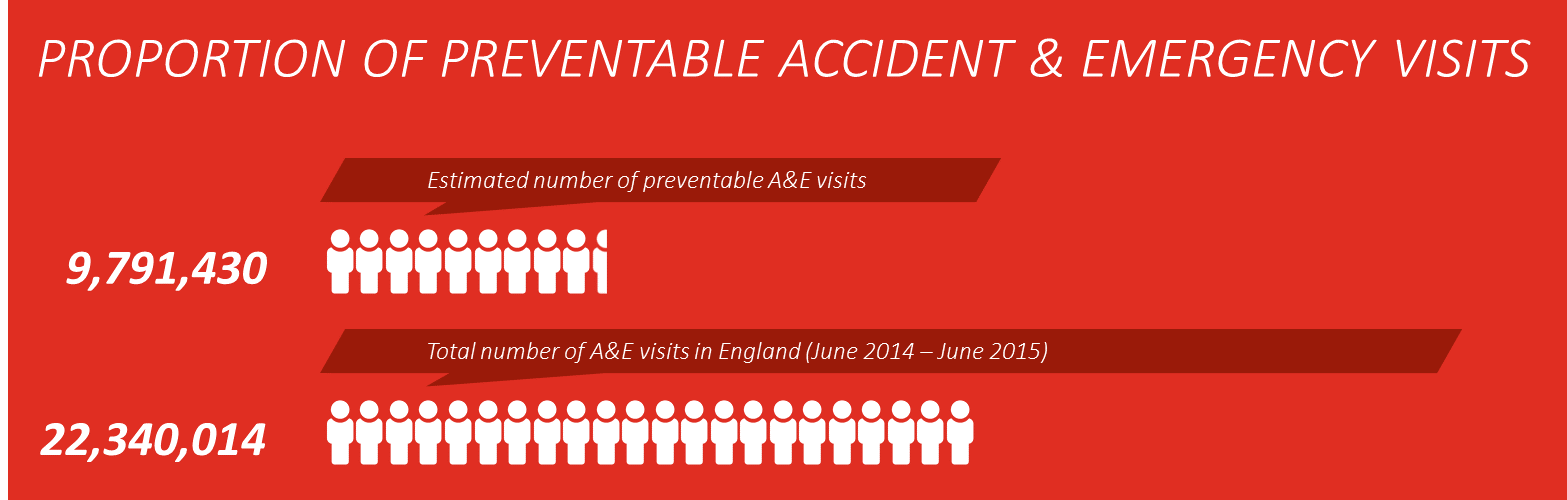
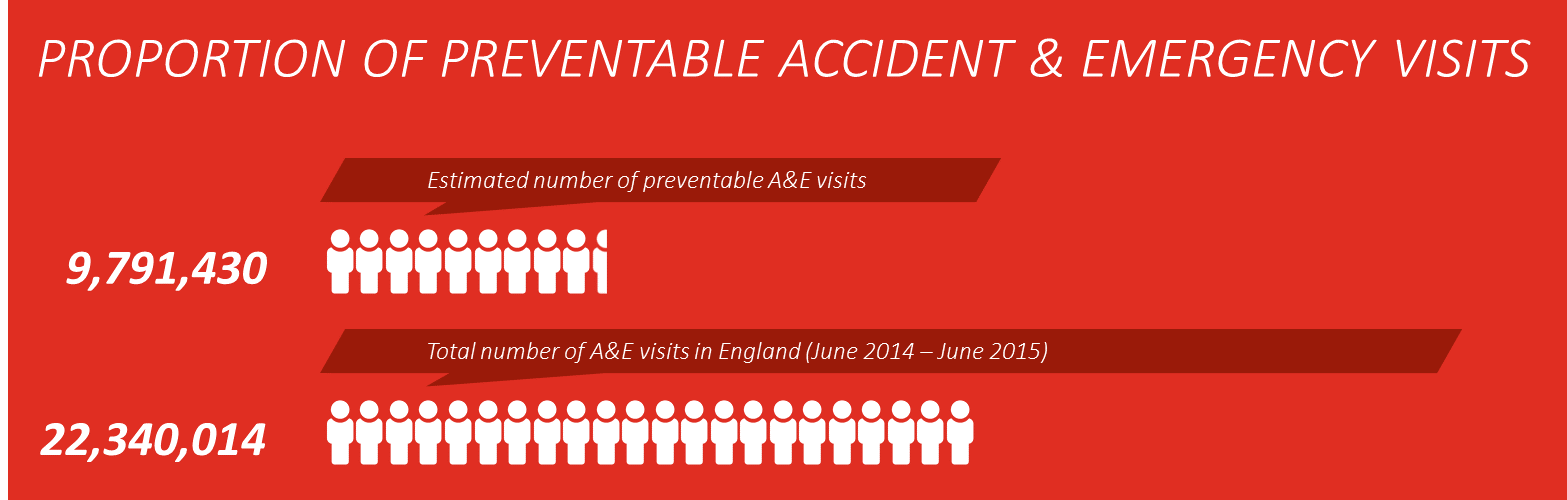
The picture that these results paints is one in which the youngest generations in society emerge as worryingly frequent and potentially erroneous users of Emergency Departments. It seems as though a small, but significant tranche of younger patients are substituting the use of GPs with A&E Departments. Based on our calculations, half of the visits to A&E made by those aged 34 or under are preventable. These account for over a third of national visits and equates to over 3.5 million visits a year.
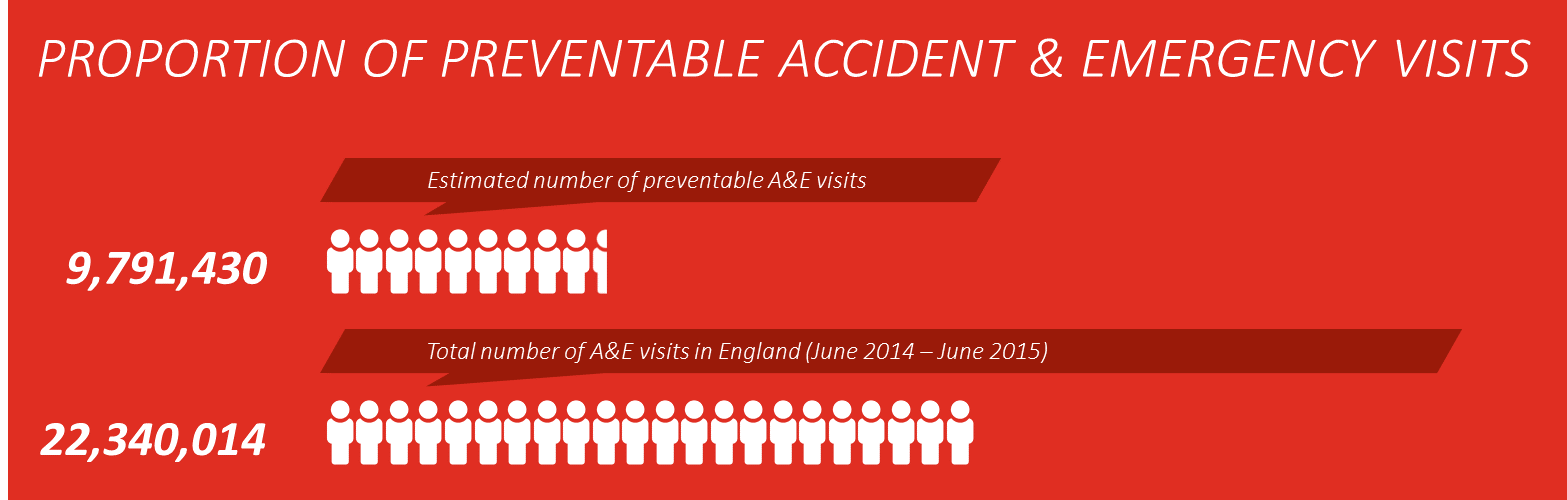
Admittedly, while our calculations are an estimated projection on national figures, even if we were to add a significant margin of error to our results the number of preventable visits would still be rather substantial. Furthermore, if we look at the main reasons for visiting Emergency Departments by age group we can see that our figures ? while surprisingly stark ? do appear to reflect the fact that a significant number of visits are not driven by emergency situations.
Two figures appear to leap out from the chart above. The first is that 21% of those aged 34 and under stated that they visited A&E because they wanted to be seen that day compared to just 10% of those aged 55 and over (who ? incidentally ? are the most frequent users of GPs). The second is that the most common reason for visiting A&E is being referred by your GP. Over a quarter of UK adults said that they had visited A&E due to a GP referral, with a further 22% stating that they had been referred by NHS 111.
Bearing in mind then that the two driving factors of visits to A&E are a lack of GP appointments on the same day and referrals to A&E by GPs, it seems logical to conclude that simply introducing a seven-day GP service would only result in further referrals to A&E ? unless it was accompanied by a significant increase in the number of GPs and resources available, which the Royal College of GPs suggested last week was unrealistic (http://bbc.in/1iriJCc). This a view shared by the vast majority of the public (68%) who believe that the move will place too much pressure on GPs.
If an extension of GP services is unlikely to relieve the pressure on Emergency Departments and does not have the support of the public, what other avenues should we be looking to explore?
Our findings suggest that generational change is responsible for the increase in pressure on hospital resources, rather than an increase in the number of health complications. Younger generations, who are used to on-demand services and information at their fingertips, are opting to bypass the GP appointment queue and head straight to hospital departments. While the vast majority of these visits are undoubtedly serious and require immediate treatment, our research shows that an alarmingly high number of them are treatable outside of hospital wards.
Perhaps the answer lies in replicating the on-demand service models of other industries in the healthcare sector. For example, high street retailers have revived their sales by offering digital channels for browsing and shopping ? providing their customers with an instantaneous and convenient method for engaging with their products. Can the same approach be applied to the healthcare sector to provide reassurance to non-acute patients and reduce the number of preventable visits? Can technology be used to better streamline or triage patients waiting for GP appointments, or can digital communication enable better resource management ? allowing patients in one area of the country to connect with under-utilised nurse practitioners or GPs in other parts of the country? Can better online resources and mobile applications engage younger generations in healthy living and drive attitudinal change towards how healthcare services are used?
We think these are interesting and important questions for the healthcare sector ? with the cooperation of other sectors ? to address. That?s why on Friday 18 September we will be presenting a research report on how technological innovation can improve healthcare provision and drive optimisation at the Connected Health Event 2015. You can find information on the conference and reserve tickets here: http://www.hti-labs-events.com/.
We hope to see you there.
Our Healthcare division provides insightful research and counsel to public health organisations, healthcare providers, pharmaceutical companies and health insurers to help improve patient outcomes, identify new opportunities and create efficiencies.
If you?d like to know more about what we can do for you, please get in touch.
* Our calculations were based on responses from 673 UK adults who had visited Accident & Emergency in the past year. We defined preventable visits as any visit that resulted in discharge without treatment or referral back to GP. For visits that were caused by non-emergency or non-referral situations (e.g. I wanted to be seen that day) or caused by illnesses that NHS Choices recommends a GP appointment for (e.g. cold or flu, stomach ache) we estimated that 50% of these appointments were preventable (i.e. non-acute). Our calculations resulted in a proportion of total visits that were preventable, which we applied to the latest statistics provided by NHS England (http://www.england.nhs.uk/statistics/tag/ae-attendances/) to arrive at our total figure of preventable appointments.